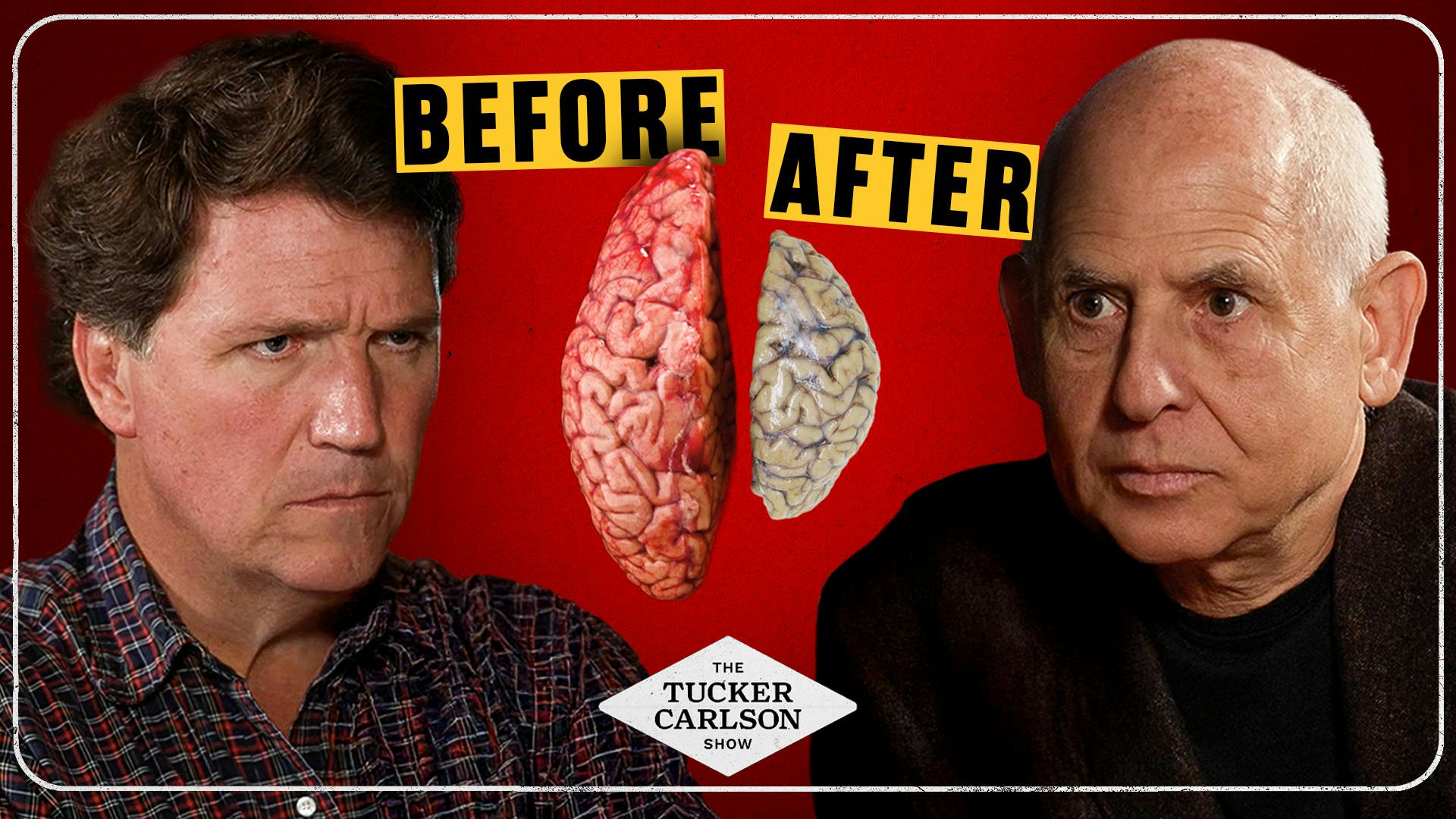
Overview of Big Pharma’s Most Dangerous Lie and the Dark Truth About Weed
This episode (Tucker Carlson Network) features psychiatrist Dr. Daniel Amen (founder of Amen Clinics) discussing brain health, the measurable harms of cannabis and other substances, societal trends that normalize brain-damaging behaviors, and a practical prevention/recovery framework he calls "Bright Minds." The interview mixes neuroscience (SPECT imaging, mitochondria, neuroplasticity), public-health commentary, clinical anecdotes (youth scans, NFL players, a child with a brain cyst), and a long list of lifestyle recommendations and supplements to protect or rebuild the brain.
Key topics covered
- SPECT brain imaging and what it shows (blood flow, mitochondrial uptake, activity patterns)
- How cannabis affects the brain: lower blood flow, reduced mitochondrial function, slowed cognition, increased risk of depression/anxiety/psychosis (especially in young users and genetically vulnerable people)
- Broader societal “lies”: normalization of marijuana, alcohol as harmless, over-prescribing opioids/benzodiazepines, under-studying video games/social media/AI effects
- Other brain insults: obesity, toxins (phthalates, sunscreen chemicals), head trauma, infections (including long COVID), general anesthesia
- Addiction and habit neuroscience (dopamine loop, frontal-lobe control vs habit centers)
- Prevention and recovery: a practical framework (Bright Minds) and concrete lifestyle interventions
- Concerns about psilocybin, kratom, and the commercialization/promotion of intoxicants
- Clinical anecdotes demonstrating that scanning the brain can reveal treatable, non-psychiatric causes of psychiatric symptoms
Main takeaways
- Heavy or early cannabis use is associated—on brain imaging and in multiple studies—with reduced blood flow/activity in learning/memory regions, mitochondrial dysfunction, and increased risks for anxiety, depression, suicide, psychosis and (potentially) dementia.
- Some genetic variants greatly increase the risk that heavy cannabis use will trigger psychosis (one gene combo cited as ~7× risk for vulnerable people).
- Brain damage from substances and other factors can be visible on SPECT scans; scanning can change diagnosis and treatment (example: a child with a cyst causing violent behavior).
- The modern normalization and commercialization of drugs (marijuana, kratom, psilocybin) can undermine public health—money and politics impede frank warnings.
- Many common lifestyle factors (obesity, poor diet, lack of exercise, sleep problems, toxins, infections) accelerate brain aging and raise dementia risk—many of these are modifiable.
- Neuroplasticity works both ways: lifestyle choices can make your brain better or worse. Interventions (behavioral, dietary, medical when needed) can improve scans and outcomes.
Notable stats and studies cited (as presented in the episode)
- Amen Clinics SPECT study on ~1,000 marijuana users: every brain region lower in blood flow/activity compared with healthy controls (mitochondrial dysfunction emphasized).
- Independent imaging study of ~1,000 young marijuana users: reduced blood flow/activity in learning & memory areas.
- Genetic vulnerability: one gene abnormality + heavy cannabis use → ~7× increased risk of psychosis for those individuals; average increased risk for users estimated at 2–4× (higher with early use).
- CDC youth mental-health data quoted: 57% of teenage girls reported persistent sadness; 32% had thought of suicide; 24% planned; 13% attempted (as cited).
- Obesity and brain volume: overweight → ~4% less brain volume (brain appears ~8 years older); obese → ~8% less (brain ~16 years older) — study from Univ. of Pittsburgh referenced.
- Marijuana under age 50 associated in a cited study with a ~600% increased risk of heart attack.
- Addiction probabilities: alcohol use → ~15% risk of addiction; marijuana use in youth → ~17%; older users → ~9%.
- Lancet review: up to 50% of Alzheimer’s disease potentially preventable by addressing modifiable risks.
Bright Minds framework — the 11 risk domains to prevent or treat
(Dr. Amen’s mnemonic "BRIGHT MINDS" — reconstructed from the interview)
- B — Blood flow (exercise, control BP, avoid substances that impair circulation)
- R — Retirement & aging (stay mentally active; learn new skills)
- I — Inflammation (diet, omega‑3s, reduce processed foods; floss/gum health)
- G — Genetics (know family risks; adopt prevention if at risk)
- H — Head trauma (prevent concussions; protect frontal lobes)
- T — Toxins (drugs, alcohol, mold, personal-care product chemicals)
- M — Mental health (treat depression/anxiety; CBT; avoid deleterious meds where possible)
- I — Immunity & infections (optimize vitamin D, treat infections, address long‑COVID effects)
- N — Neurohormones (test/optimize testosterone, thyroid, etc.)
- D — Diabetes (control weight, blood sugar)
- S — Sleep (treat sleep apnea, prioritize restorative sleep)
Practical, actionable recommendations (what listeners can do)
- Ask before you act: “Is this good for my brain or bad for it?” make choices based on that.
- Avoid or limit heavy/early cannabis use—especially for teens and young adults.
- Limit alcohol; recognize both alcohol and marijuana have addiction risk and long-term harms.
- Avoid kratom (described as an addictive, unregulated opiate agonist).
- Be cautious with unregulated/“enthusiastic” use of psilocybin—medical contexts are not the same as recreational use; microdosing risks are unstudied/wild west.
- Protect sleep; screen and treat sleep apnea.
- Exercise regularly: aerobic + coordination + strength to boost blood flow and brain health.
- Reduce inflammation and processed foods; favor a Mediterranean/FAT-based (healthy fat) diet pattern (fish, leafy greens, nuts).
- Maintain healthy weight; losing excess weight helps brain structure and function.
- Optimize vitamin D; check levels and supplement sensibly.
- Improve oral health (floss): gum disease/infections promote systemic inflammation.
- Get annual bloodwork including ferritin (donate blood if iron high).
- Consider evidence-backed supplements when appropriate: omega‑3s (fish oil), curcumin (turmeric component), saffron (mood/memory), zinc, quercetin (anti-inflammatory) — discuss with your clinician.
- Manage automatic negative thoughts: cognitive strategies (write thoughts down, question them, turn to opposites), CBT-style tools, name your “mind” to gain distance.
- If you or someone has a sudden change in behavior, consider medical/neuro workup (imaging) — psychiatric symptoms can be caused by structural lesions, infections, etc.
Clinical anecdotes & illustrative cases
- NFL player Julius Randle: cannabis use harmed his presence and relationships; he performed better after quitting and brain-focused rehab.
- Young patient with "toxic" SPECT scan where scanning revealed marijuana/drug effects (used to show teens the objective brain impact).
- Nine-year-old godson with violent behavior: SPECT/MRI revealed a large temporal-lobe cyst; neurosurgery reversed the behavioral decline and improved outcome.
- “Nancy” (frontotemporal dementia): intensive Bright Minds-style intervention + hyperbaric treatment produced measurable scan improvement and extended home care.
Risks highlighted for specific substances
- Cannabis: impaired cerebellar function (coordination/thought speed), reduced blood flow/mitochondrial activity, increased risk of psychiatric illness (esp. with early onset), potential increased dementia risk with long-term use.
- Psilocybin: therapeutic promise in controlled settings but recreational use can trigger psychosis and hallucinations—ER visits have risen; dosing in trials is controlled and not comparable to recreational practices.
- Kratom: marketed as benign but is an opiate agonist, addictive, and linked to worsened brain scans/clinical outcomes in cases described.
- Alcohol: widely normalized but linked to brain volume loss, cancer risk, and other harms; not a benign “health food.”
Notable quotes / memorable lines (paraphrased)
- “If your brain is not right, you’re not right.”
- “Teach people to love their brain first — then they’ll be more likely to avoid hurting it.”
- “Neuroplasticity goes both ways: whatever you repeat, you wire in.”
- “Ask the question: Is this good for my brain or bad for it?”
Caveats & context
- Many of the numbers and study findings were presented verbally by Dr. Amen; listeners should consult primary literature or clinical guidance for medical decisions.
- Dr. Amen’s clinical approach heavily emphasizes SPECT imaging; SPECT use in psychiatry is debated among clinicians and may not be standard practice everywhere.
- The episode blends clinical evidence, opinion, and social commentary; treat policy and clinical recommendations as subject to broader scientific review.
Bottom line
This episode is a call to prioritize brain health: avoid or limit brain-damaging exposures (heavy cannabis use, alcohol, kratom, toxins, processed food, head trauma), adopt lifestyle practices that improve blood flow, reduce inflammation, and support hormones/sleep, and use cognitive strategies to manage thinking. Dr. Amen argues many harms are measurable (on imaging) and preventable/reversible if addressed early—and warns that the commercialization and normalization of psychoactive substances is a major public-health threat, especially to youth.